The Rise of Korean Dental Implants: A Global Success Story
October 26, 2025Abstract:
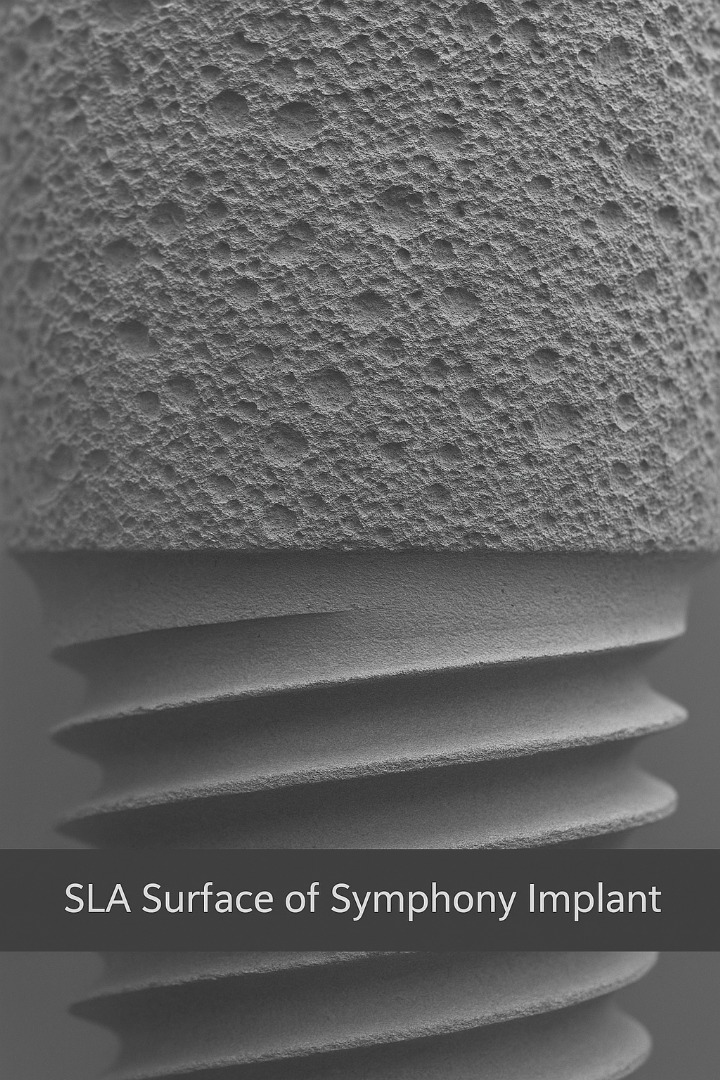
Surface treatment is one of the most important determinants of dental-implant success. Among available technologies, SLA (Sandblasted, Large-grit, Acid-etched) has the strongest and most consistent clinical evidence for promoting rapid and reliable osseointegration. This article summarizes the biology behind surface effects, presents comparative clinical evidence (including outcomes versus RBM/resorbable blasting media surfaces), and explains why Symphony Implant uses an SLA surface to maximize early bone contact, stability, and long-term success.
- Why implant surface matters
When an implant is placed, the implant surface is the immediate interface with blood, proteins and bone cells. Surface topography and chemistry strongly influence:
- protein adsorption and clot stability,
- osteoblast attachment and differentiation, and
- mechanical interlocking (primary stability → secondary, biological stability).
A moderately rough surface increases surface area and micro-pockets where bone can grow into the implant, accelerating bone-to-implant contact (BIC) and reducing early micromotion that can cause failure.
(Broad literature reviews and animal/human studies show roughened surfaces outperform polished machined surfaces in BIC and early stability.) PMC+1
- What SLA (Sandblasted, Large-grit, Acid-etched) is — and why it works
SLA is a two-step process:
- Sandblasting with large particles creates a macro-roughness that increases mechanical interlocking.
- Acid etching (typically with strong acids) creates micro-roughness that promotes cellular attachment and differentiation.
The combination produces a hierarchical topography (macro + micro), which is widely reported to enhance osteoblast response, increase BIC, and support earlier functional loading compared with smooth or single-step surfaces. PMC+1
- Evidence: SLA clinical performance and survival
Multiple clinical and retrospective studies report high survival rates and favorable marginal bone behavior for SLA implants:
- Several clinical cohorts and reviews report SLA implant survival rates >95% over typical follow-up periods, including 2–5 year studies. PMC+1
- SLA surfaces have repeatedly demonstrated strong early stability and are commonly recommended for immediate or early loading protocols when indicated by case selection. PMC
- SLA versus RBM (resorbable blasting media) — what the data say
RBM (often blasted with calcium phosphate or other resorbable particles) is another widely used roughening method. Comparative studies between SLA and RBM show the following patterns:
- Marginal bone loss (MBL): Recent prospective cohort data indicate SLA implants are associated with equal or lower marginal bone loss than RBM implants when macro-design is controlled. One 2023 study found SLA had lower MBL compared with RBM under similar implant geometries. PMC+1
- Survival / success rates: Large retrospective analyses and pooled data (thousands of implants) suggest both surfaces achieve high survival, but several reports show a small advantage in survival or lower early failure risk for SLA in aggregated datasets. For example, analyses pooling thousands of implants have reported superior BIC and biomechanical integration metrics for SLA vs RBM. ResearchGate+1
- Variable findings and context: Not all studies show a clinically meaningful difference in long-term survival; some randomized trials report no significant difference between certain SLA variants and other rough surfaces for specific endpoints. Outcomes can depend on implant geometry, surgical protocol, patient biology, and follow-up duration. PMC+1
Bottom line: SLA has a stronger and more consistent track record for promoting higher BIC and lower early marginal bone loss than many RBM systems—particularly when early stability and bone quality are concerns—although both surface types can achieve excellent long-term survival when used correctly.
- Key quantitative takeaways (what clinicians ask)
- Survival: SLA implants routinely report ≥95% survival in 2–5 year clinical series. PMC+1
- Bone-to-implant contact / biomechanical metrics: Histologic and micro-CT studies repeatedly show higher BIC ratios and greater biomechanical fixation for SLA compared with many other roughening methods (including RBM) in preclinical and retrieval analyses. PMC+1
- Marginal bone loss: Prospective comparisons indicate SLA tends to produce equal or reduced MBL vs RBM when implant macro-design is held constant. PMC+1
(Note: exact percentages and effect sizes vary by study design, cohort, follow-up time, and implant geometry. Where randomized, controlled long-term trials exist they sometimes show smaller differences; however, pooled clinical experience and histologic data favor SLA for earlier, stronger osseointegration.) ResearchGate+1
- Why Symphony Implant uses SLA
Symphony Implant’s fixtures are finished with a controlled SLA surface engineered in Korea under strict process control. This choice is driven by the clinical goals of:
- maximizing early bone contact (higher BIC),
- enabling predictable early/standard loading protocols, and
- minimizing marginal bone loss risk in challenging bone types.
By using SLA, Symphony aligns its product with a surface treatment that has one of the strongest evidence bases for promoting reliable osseointegration. (See representative clinical studies and cohort reviews cited above.) PMC+2PMC+2
- Practical recommendations for clinicians
- Match surface choice to clinical indications. SLA is an excellent default for general use, especially when early stability or compromised bone quality is a concern. PMC
- Consider macro-design + surface together. Thread form, tapered vs straight body, and platform design interact with surface topography to determine stability and load distribution. journalofosseointegration.eu
- Surgical and prosthetic protocol matter. Even the best surface cannot overcome suboptimal surgical technique, poor primary stability, or improper loading. Follow evidence-based protocols for drilling, insertion torque, and loading timing. PMC
- Conclusion
Surface engineering is not an afterthought — it is central to predictable implant dentistry. SLA remains one of the best-documented surface treatments for creating quick, strong bone integration with favorable marginal bone outcomes. Symphony Implant’s SLA surface therefore represents a deliberate, evidence-driven choice to provide clinicians with implants that support faster osseointegration, dependable stability, and long-term success.
References (selected)
- Kim SB et al., Comparative Study of Early Loading of RBM and SLA Implants — clinical outcomes and survival (retrospective/cohort). PMC
- Five-year radiographic follow-up of SLA implants (Korean cohort). PMC
- Nemati M., Comparison of marginal bone loss in SLA and RBM implants (2023) — prospective cohort showing lower MBL with SLA. PMC+1
- Jeong KI et al., histologic analysis of RBM surfaces and comparisons with other surfaces. Semantic Scholar
Large pooled analyses and reviews comparing SLA vs RBM across thousands of implants. ResearchGate+1